Understanding and Eliminating Disparities in Maternal Health Outcomes, Part II
By: Christine H Morton, PhD | 0 Comments
Today's post is the second one on disparities in maternal health care by regular Science & Sensibility contributor, Christine Morton, PhD, who is a medical sociologist and has researched and written about disparities in maternal health for many years. Today, Christine takes a look at why women of color in the United States are facing a widening gap in maternal health outcomes and what some of the underlying factors might be. This is part two of a two part series that looks at the research and examines what might need to change. - SM
Are public health and obstetric perspectives providing us with the best paradigms for understanding and eliminating racial-ethnic disparities in maternal health outcomes? In my last post, I reviewed a typical public health study, which looked at maternal mortality by race, ethnicity and nativity, based on U.S. death certificate data from 50 states and two cities: NYC and Washington, DC.1

Photo Image Creative Commons Linda Dias, Photos
Documenting outcomes, while important, is only part of the answer to understand why racial-ethnic disparities exist, persist, and widen. Even more, we can't begin to eliminate disparities until we have a better understanding of how different groups of women experience the birth process. By process, I mean the local context in which women experience pregnancy and give birth, the pattern of interventions and decision-making, the attitudes and behaviors of healthcare clinicians and childbearing women. One of the best methodologies for examining local contexts of birth is ethnography, in the tradition of such classics as anthropologist Brigitte Jordan's Birth in Four Cultures: A Cross-Cultural nvestigation of Childbirth in Yucatan, Holland, Sweden and the United States (1978) and sociologist Nancy Stoller Shaw's Forced Labor: Maternity Care in the United States (1974.) Only recently are social scientists turning their ethnographic lenses to current U.S. hospital childbirth settings, and I will highlight some of these projects in future posts.
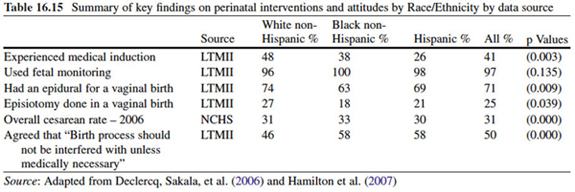
Eugene Declercq, Mary Barger, and Judith Weiss2 review the evidence for disparities among five major interventions in childbirth: induction, electronic fetal monitoring, epidurals, episiotomy, and cesarean section. They use data from multiple sources, 'reflecting the fragmented nature of data systems related to the birth process.' The birth certificate in many states has an extended worksheet, but the quality and accuracy of many elements on the birth certificate is a serious issue. The best way to look at administrative data on pregnancy and childbirth is to have a LINKED data set that matches Birth Certificate data with Hospital Discharge Data, thus allowing for risk stratification by age, parity, etc.
DATA SOURCES ON PREGNANCY and CHILDBIRTH
| Data Source |
Agency |
What it provides |
Used in this paper |
| Birth certificate |
National Center for Health Statistics (NCHS) |
Overall national trends and disparities by race/ethnicity |
Yes |
| Hospital discharge data (ICD-9/10 codes) |
National Hospital Discharge Survey |
Episiotomy use |
Yes |
| Massachusetts natality data |
MA Dept of Public Health |
Includes method of payment |
Yes |
| Listening to Mothers II Survey |
Childbirth Connection |
National retrospective survey of 1573 women who gave birth in 2005 (weighted for representativeness) |
Yes |
| Pregnancy Risk Assessment and Monitoring System (PRAMS) |
Centers for Disease Control and Prevention |
Population based survey of postpartum women conducted annually in 39 states |
No - only one question related to birth: 'When was your baby born?' |
Induction
Declercq and colleagues state that 'rates of labor induction have more than doubled over the last 15 years in the United States,' and they review the geographic variability observed in this procedure - between states, within states, and among different types of hospitals. The authors speculate that the rapid increase in induction rates, especially 'elective inductions under 41 weeks gestation may have contributed to the shift in the gestational age distribution of births, with 39 weeks now being the most common gestational age.'
Rates of induction by race/ethnicity vary by data source. National birth certificate data from 2005 show that 'Regardless of parity, rates were highest among white non-Hispanic women, lowest among Hispanic women, with black non-Hispanic women falling in between. First time mothers in each group have higher rates than multiparous mothers.'
Listening to Mothers II (LTMII) asks women whether they attempted to induce labor, whether their labor was medically induced and whether it was successful (i.e., no cesarean). LTMII reported a higher overall rate of induction than the national birth certificate data (34% vs. 22%), in part because LTMII asks about a greater variety of methods, and because national birth certificate data only report those inductions that result in labor. While techniques used to induce labor did not differ by race/ethnicity, LTMII found that Hispanic women who had given birth before had highest rates of attempted and successful induction (43% and 38%, respectively) compared to White women (39% and 33%) and Black women (29% and 22%) who had given birth before. Regardless of parity, White women were more likely than Black or Hispanic women to try to self-induce (25% vs. 17% vs. 18%).
The authors also look at evidence for induction at 41+ vs. 42+ weeks gestation, but the data presented from LTMII and birth certificates does not include gestational age at induction. This data element is on the birth certificate but is highly subject to error and missing values.
Cesarean Delivery
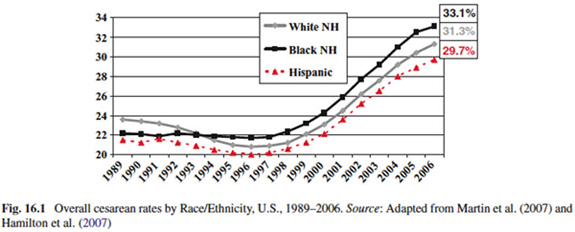
We know that cesarean rates have rapidly increased in the U.S. and that this rate has occurred among all racial/ethnic groups. However, in this figure, Declercq and colleagues show that Black women had lower cesarean rates than White women until 1994, when they surpassed all groups, reaching 33.1% in 2006, compared to White women (31.3%), and Hispanic women (29.7%). One reason for this is that Black women never experienced the decline in cesarean births the other groups did due to the rise in vaginal birth after prior cesarean (VBAC).
Black women have higher rates of cesarean at nearly every age group, and this is true among the three time periods examined (1991, 1996, 2005) and among every level of education. Because the national data has limited variables to measure social status, Declercq and colleagues looked at Massachusetts data by payer. Again, regardless of whether they had private or public insurance, Black women had higher rates of cesarean than White or Hispanic women.
Conclusion
Declercq and colleagues have made a valuable contribution to the public health literature by pointing out the gaps in public health surveys and summarizing what is known about its evidence base, current practice and associated health disparities. They conclude:
Three clear findings emerge:
(1) while there has been considerable research on each of these interventions, actual practice is not consistently related to its associated evidence base;
(2) randomized trials have not examined the relationship of these interventions and disparities in outcomes; and
(3) in all cases but fetal monitoring, which is virtually universally applied, there are differences in the application of the interventions to mothers from different race/ethnicity groups. However, there is also no clear pattern that would suggest that one group is more likely than any other to receive evidenced-base care.
Discussion
So back to the opening question - Are public health and obstetric perspectives providing us with the best paradigms for understanding and eliminating racial-ethnic disparities in maternal health outcomes? In light of the variation among common childbirth procedures (interventions) like induction and cesarean, and with research showing that African American women are more likely to have cesareans, 3-5 yet are less likely that White women to agree that the birth process should not be interfered with unless medically necessary, how do we understand what is happening in clinics and labor units across the country?
Clinicians are beginning to realize that quantitative data is only the first step toward changing behaviors, and acknowledge that health care culture drives much of this practice variation.6 Yet most clinician researchers are untrained in the methods best suited to discovering how to maximize quality improvement efforts - ethnography and qualitative research. Donald M Berwick (Institute for Healthcare Improvement) has argued for a wider embrace of methodologies beyond the 'gold standard' randomized control trial, to assist quality improvement efforts in health care. In particular, he informs his clinical colleagues that approaches such as 'ethnography, anthropology, and other qualitative methods are not compromises in learning how to improve; they are superior'.2
Clinicians, public health researchers (and maternity care advocates) have long relied on population data to make the case that evidence-based care can improve maternal and infant health outcomes. Yet every childbirth educator and doula knows the value of the story - which includes the mechanisms (how things work in practice) and context (local conditions, including actions and meaning, that influence the outcomes of interest). Systematically combining good epidemiological data with compelling accounts of the childbirth experience by all participants is the next research frontier we must cross in our quest to improve the quality of care and outcomes for all women and their babies.
References
1. Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Race, ethnicity, and nativity differentials in pregnancy-related mortality in the United States: 1993-2006. Obstetrics and gynecology. Aug 2012;120(2 Pt 1):261-268.
2. Declercq E, Barger M, Weiss J. Contemporary Childbirth in the United States: Interventions and Disparities. In: Handler A, eds. Reducing Racial/Ethnic Disparities in Reproductive and Perinatal Outcomes: The Evidence from Population-Based Interventions: Springer Science+Business Media; 2011:401-427. Accessed online: http://www.springer.com/public+health/book/978-1-4419-1498-9
3. Braveman P, Egerter S, Edmonston F, Verdon M. Racial/ethnic differences in the likelihood of cesarean delivery, California. Am J Public Health. May 1995;85(5):625-630.
4. Getahun D, Strickland D, Lawrence JM, Fassett MJ, Koebnick C, Jacobsen SJ. Racial and ethnic disparities in the trends in primary cesarean delivery based on indications. American Journal of Obstetrics and Gynecology. Oct 2009;201(4):422 e421-427.
5. Roth LM, Henley M. Unequal Motherhood: Racial-Ethnic and Socioeconomic Disparities in Cesarean Sections in the United States. Social Problems. 2012;59(2):207-227.
6. Main E, Morton C, Hopkins D, Giuliani G, Melsop K, Gould J. Cesarean Deliveries, Outcomes, and Opportunities for Change in California: Toward a Public Agenda for Maternity Care Safety and Quality. Palo Alto, CA: California Maternal Quality Care Collaborative;2011. Available online: http://www.cmqcc.org/white_paper
Published: September 13, 2012
Tags
Maternal Infant CareListening to Mothers SurveysLearning OpportunitiesConnected ChildrenChristine Morton PhDBirth AdvocateEugene Declercqbetter birth outcomesbetter pregnanciesMother-baby bonding improvementRacial Disparities In Maternal Mortali