The Maternal Quality Landscape-Part Three, Segment Two: How do we measure AND achieve it?
By: Christine H Morton, PhD | 0 Comments
Perinatal Measure Case Study: Elective Deliveries <39 Weeks
The <39 weeks measure is designed to capture the percentage of elective vaginal or cesarean deliveries at greater than or equal to 37 and less than 39 completed weeks of gestation. Elective in this sense means "scheduled and having no medical indication."
Background: How did <39 Weeks become an Issue?
The seeds of the <39 weeks measure were planted over a decade ago. One early alarm bell was the finding in 2002 that average length of gestation was shifting downward, with 39 weeks becoming the most common gestational age among babies rather than 40 weeks (Davidoff et al., 2002). Figure 1 shows how the distribution of singleton live births in the US has shifted since 1992 (Fleishman 2011). At the same time, research was emerging which showed that babies born at 'term' but at less than 39 weeks' gestation, had poor outcomes.

Effects of ED<39 Weeks on Babies and Mothers
Researchers have demonstrated significant variation in the health of babies born during the five-week window considered "full term" (Fleischman, Oinuma, & Clark, 2010). And, as Amy Romano writes in a recent S&S blog post, new research suggests these early term births may be associated with emotional health costs for mothers.
Most providers do not see a lot of bad outcomes in infants who are born during this time, so many had been unaware of the growing literature suggesting a problem. However, overall, there has been an increase in NICU admissions of infants that are considered "term" but are born prior to 40 weeks (Clark 2009; Morrison 1995; Madar 1999; Tita 2009). Anecdotally, lactation consultants note that babies born less than 40 weeks seem to have an increased risk of breastfeeding problems. They are called "imposter babies," because they have difficulty nursing like a full term infant despite having the appearance of one.
To address the growing concern about these avoidable harms to babies born prior to 39 weeks, a public awareness campaign was spearheaded by the March of Dimes, which included a re-definition of preterm births.
Shifting definitions of "term" and "preterm"
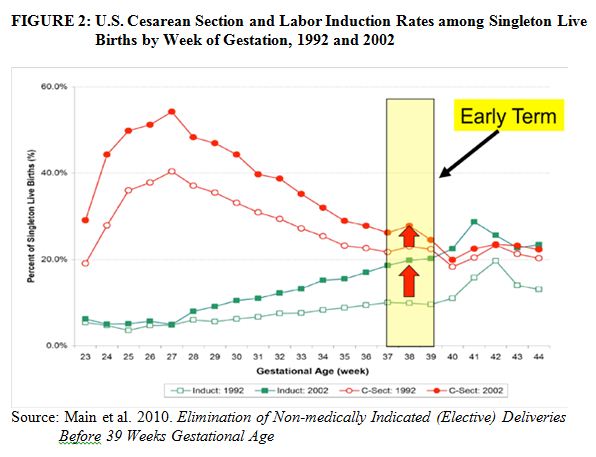
Definitions of prematurity have a complex history. In 1948, the World Health Assembly adopted a definition of "prematurity" that tied birth weight to gestational age; an infant was considered premature IF it weighed less than 2500 grams (~5.5lbs) AND/OR estimated gestational age was less than 38 weeks (Drillien, 1974). However, many (healthy) babies were classified as premature who were not actually born prior to 38 weeks, and babies who were less than 38 weeks but over 2500 grams were misclassified as not premature. Researchers recognized that although there was a relationship between gestational age and newborn weight, these two categories did not map directly onto each other. Subsequently, new classification schemes were developed that subdivided infants into separate categories based on prematurity and weight. Definitions for pre-term (less than 37 weeks); term (37 through 41 and 6/7 weeks); and post-term (42 weeks or more) were developed and became well-established in obstetric practice. Additionally, in recent years researchers have proposed new sub-categories. In particular, there was a further distinction among the pre-term births for those occurring between 34-36 completed weeks (previously referred to as near-term): "Late preterm" (Engle, 2006) and those occurring between 37 and 39 completed weeks: "Early term " (Fleischman et al., 2011) (See Table 1). The observed rise in births occurring in the time frame that was technically considered "term" - births occurring in the 37-39 week range - can be seen in Figure 2.

How the Upper Limit was Defined as 39 Weeks
Selecting gestational ages between 37 and 39 completed weeks as a target for a quality measure was based on research briefly outlined above as well as clinical consensus that babies born at less than 39 completed weeks have worse outcomes than those born after; but it was never designed to be a prescribed or recommended delivery goal for all babies.
A large body of literature, summarized in the California Maternal Quality Care Collaborative (CMQCC)/March of Dimes Toolkit (Main et al. 2010), shows that babies born before 39 weeks are at increased risk for NICU admission and sepsis and are more likely to need a ventilator, among other problems.
However, research also suggests that babies born after a certain point may be more likely to be stillborn. In particular, the mortality rate increases for babies born after 42 weeks gestation, although the causes of this phenomenon are still unclear. Mortality in post-term infants has not been linked definitively to prolonged pregnancy itself but may be linked to fetal growth restriction and fetal deformities. Currently, there is debate about whether or not elective induction at 42 weeks is better than expectant management (Mandruzatto et al., 2010).
It is important to remember that 39 weeks was not chosen because it is the optimal time for a baby to be born; indeed it seems that very few pregnancies last long enough to enter a time that may be sub-optimal. Instead, 39 weeks was chosen because research has shown it is the point at which the baby appears to suffer little additional harm from being outside the uterus as opposed to inside of it. There is some evidence to suggest that for scheduled repeat cesareans, delivery between 39-40 weeks is optimal for neonatal outcomes.
[Tomorrow's post explores how hospitals identify and document <39 weeks births including use of The Joint Commission's specifications for calculating perinatal quality measures To read segment one, go here. To read this series from the beginning, go here.]
Published: December 27, 2011
Tags
Lamaze EducatorsMaternity CareMaternal Infant CareMaternity Care QualityCMQCCKathleen PineNational Quality ForumBan On Early Elective CesareanOnline StoreBan On Elective Deliveries Before 39 WeeksMaternal Quality CarePerinatal Core Measure Set