Rigging the Election: When it comes to elective induction, are women asking for it?
By: Amy M. Romano, RN,CNM | 0 Comments
There is a growing movement, backed up by evidence, practice guidelines, and efforts by agencies including the March of Dimes, the Institute for Healthcare Improvement and the Joint Commission, to reduce elective inductions, especially those occurring before 39 completed weeks of gestation.
Media coverage of these efforts tends to frame the problem as too many women asking for early delivery with no medical reason and the solution as hospitals 'saying no' to these women. But this woman-blaming paradigm is simplistic and flawed. New research shows that, not only have maternity care providers failed to convey the risks of early delivery to women, they may be offering or recommending elective deliveries despite the risks, and telling women they have a medical reason for induction but documenting the inductions as 'elective'.
First, the evidence that educating women does help.
As reported in the July/August issue of the American Journal of Maternal/Child Nursing, researchers at St. John's Mercy Medical Center in St. Louis, MO, studied the effect of a 40-minute educational intervention given in the context of hospital-based Lamaze classes. The intervention was an educational module about elective induction incorporating evidence and professional practice guidelines, taught along with the otherwise-unchanged Lamaze class curriculum. Researchers compared the elective induction rates between attendees and nonattendees in the 7-month period following the introduction of the new module. The content of the educational model was straightforward:
Specific risks of elective induction presented during the class included cesarean birth with longer postpartum recovery, pain, and potential complications as well as other associated risks such as longer labor, use of pharmacologic agents and their effects on the mother and fetus, and neonatal morbidity. Benefits included advance planning and timing with personal schedules. (p. 190)
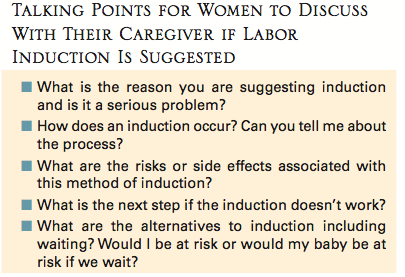
Women were also given 'talking points' to discuss with their provider if induction was recommended.
The intervention appeared to be very effective. The elective induction rate was about 37% in both attendees and nonattendees before the intervention and in nonattendees after the intervention. But 28% of women who attended the classes that included the educational content had elective inductions, a significant reduction indicating that the hospital would only need to educate about 11 first-time mothers to prevent one elective induction.
But, you might say, that still leaves more than 1 in 4 first-time mothers having electiveinductions. What else might be driving this besides lack of education? Well, it might be this: the researchers also discovered that nearly 70% of women were offered elective induction by their doctors. And, not surprisingly, women whose doctors offered them elective induction were far more likely to choose elective induction, whether or not they were exposed to the educational intervention. In fact, the magnitude of the difference was much greater than with educational content. Roughly speaking, doctors would have to refrain from offering elective induction to just three first-time mothers to prevent one elective induction.
Prior to the educational intervention, when the hospital leadership were considering how to decrease the use of elective induction, most doctors believed that the problem was that uninformed women were asking for it, an assumption turned on its head by the research findings. In postpartum surveys, three-quarters of women who had 'elective' inductions indicated that the physician suggested the option compared with only 25% of women who indicated that they initiated the request themselves. Class attendance had an influence on whether women chose to act on the option of elective induction, but the difference wasn't huge. About 38% of women who attended the class and whose doctors offered elective induction chose the option, compared with 50% of those who were offered elective induction but didn't attend the class.
The researchers conclude:
Although education provided in prepared childbirth classes can be helpful for women in making the choice of whether or not to have their labor electively induced, the physician is a powerful influence... It is possible that patients perceive the offer of the option for elective induction as a recommendation that they actually have the procedure, particularly if they are told they are due now, overdue, or their baby is getting too big. (p. 193)
And therein lies the problem: it turns out many women having 'elective' inductions think they're having medically indicated inductions. In a follow-up study by the same research team, published in the current issue of the Journal of Perinatal Education (full-text available to Lamaze members), the researchers report more of their findings from postpartum surveys as well as data gleaned from reviewing the medical records of each woman after delivery. They write:
The most significant discrepancy between the medical record and patient perception was related to macrosomia as an indication. For example, based on the medical record, macrosomia was the indication for 26.7% of inductions; however, 39.9 of patients noted that their physician told them they needed to be induced because 'my baby was too big.' The next most common reason women believed they had an induction was that they were 'due now or overdue' (20.3%), yet only 35 women (6.4%) who had an elective induction were 41 completed weeks of gestation and none were more than 41 3/7 weeks. The majority of women who indicated they were induced for being 'overdue' were only 1 to 4 days past their estimated due date. (p. 28)
So what's the take-home of all of this? How do we rein in the overuse of elective induction? Clearly, childbirth education that specifically addresses the risks, benefits, and evidence-based indications for induction helps. As we have seen, fewer women exposed to this educational content will choose induction. Researchers also found that women who had inductions were more likely to have reported feeling prepared and having the reality match up with their expectations if they had taken the classes. They were also less likely to report not knowing why they were induced compared with women who were induced but didn't take the class. In other words, the class helped women have more fruitful conversations with their care providers.
But it is clear from this research - the first to explore these issues in depth with a combination of qualitative and quantitative approaches - that we have to change provider beliefs and practices to have a meaningful impact on induction rates. It's time for more research on what happens behind the closed doors of prenatal visits, and for clear standards that tell doctors it is not okay to offer a major medical (often turned surgical) procedure to women as if it was benign or beneficial.
Published: September 23, 2010
Tags
InductionInformed ConsentLabor/Birth