Maternal Obesity from All Sides
By: Kimmelin Hull, PA, LCCE | 0 Comments
[Editor's note: This week and next on Science & Sensibility, we will discuss the issue of maternal obesity. With increasing numbers of overweight and obese women approaching pregnancy, labor and birth, complication and intervention rates are sky rocketing in this population, in sometimes controversial ways. This series of posts will attempt to answer the ultimate question: how do we tenderly care for these women, employ evidence-based practices, and still support and honor normal birth whenever possible?]
Globesity: A World-Wide Epidemic
Maternity care providers bemoan the increased risks associated with caring for overweight and obese pregnant women. The recipients of their care feel unfairly judged, overly intervened-upon and ghettoized for their body habitus. As this issue continues to grow, maternity care providers, doulas and childbirth educators need to find a way to interact with these women with equal amounts of compassion and scientific evidence. And the evidence, in and of itself, is sometimes controversial.
As it turns out, maternal overweight and obesity isn't just an American thing anymore. The World Health Organization has made a surveillance tool available on their website, where you can view charts, graphs and maps detailing the rates of adult obesity by country. Here in America, nearly 36% of adults are obese, including 1 out of 3 women. The UK reports a similar rate, with 34% of adults considered obese, including 1 out of 5 women. And pregnant American women are found to be obese 18-38% of the time.
While different countries sometimes use different methods to categorize weight status, the Body Mass Index calculator is most commonly employed:
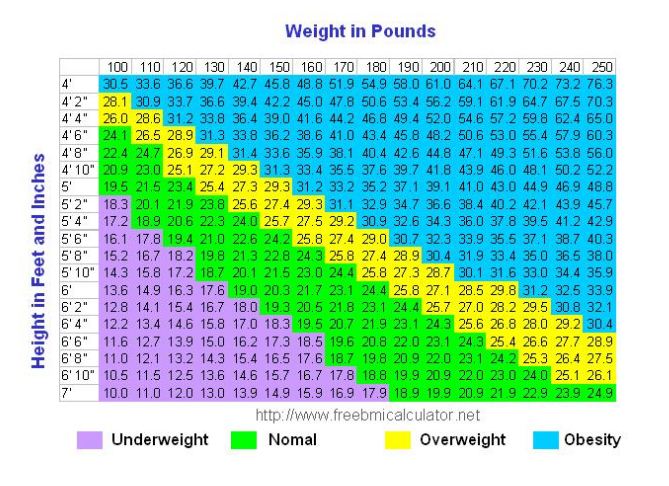
The problem with using BMI as a body weight categorization tool, is that it does not take into account bony structure, muscle mass or percentages of lean mass compared to adipose tissue. At best, Body Mass Index is a crude measure of health. However, academic literature that analyzes weight in relation to pregnancy outcomes typically uses BMI (pre-pregnancy, first prenatal appointment weight or weight at time of delivery) as a primary indicator for study group categorization.
Not only do studies use BMI to include or exclude study participants, but reports have recently emerged that some medical practices are also using BMI as a screening tool: for either accepting or rejecting patients altogether.
The Baltimore Sun recently reported on a slowly emerging trend in southern Florida, in which some maternity care practices are turning away potential new patients, if they weigh more than, say, 200 pounds. Other doctors practicing in the same area admonish their colleagues for maintaining such policies, despite the increased risk for pregnancy, labor and birth complications many in the industry believe to be an inherent part of attending pregnant women of size.
Other obstetricians, like Dr. Cynthia Maxwell at the University of Toronto Department of Obstetrics & Gynecology, are implementing clinical changes with the aim to improve treatment of and outcomes for overweight expectant mothers, as outlined in this SOCG clinical practice guideline (for which Dr. Maxwell was a principal author).
What the Evidence Shows: Risks Associated with Maternal Obesity
The basis for heightened concern'whether fueling the exclusion of certain women from their practices, or adopting new approaches to their patient care in response to the growing obesity epidemic'is in the list of complications that are known to coexist with maternal overweight, obesity and morbid obesity. It should be noted that these weight categories are not all equivalent, and that many of the risk factors we will cover here, and in subsequent posts, become riskier the more overweight or obese an expectant woman is.
In Dr. Tahir Mahmood's article, Review: Obesity and pregnancy: an obstetrician's view'a compilation of statistics from twenty different papers on the subject (British Journal of Diabetes and Vascular Disease 2009; 9: 19-22)'Table 1provides a an overview of some of the problematic conditions that can be associated with pregnancy in the overweight and obese population:
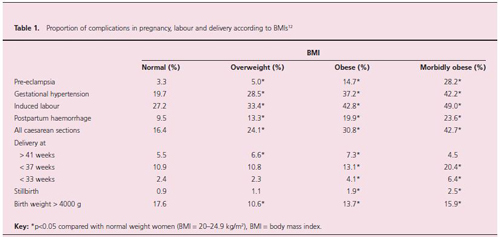
Other concerns, not listed in this table, but discussed elsewhere in Mahmood's aricle, as well as in other recent literature include:
-gestational Diabetes (GD)
-thromboembolism
-fetal macrosomia (birth weight >4,000g)
-difficulty fighting postpartum infections
-maintained overweight/obesity between pregnancies
-prolongation of pregnancy/increased likelihood to deliver postdates
-other short and long term impacts on fetus/infant/child (neural tubes defects, lifetime increased risk of diabetes and obesity)
-increased risk of stillbirth
-increased risk of maternal mortality
-postpartum hemorrhage
Complicating this issue beyond the fear factor of increasing a woman's risk of, say, postpartum hemorrhage or fetal loss is the fact that statistically, the morbidities associated with maternal weight are less than a slam dunk. While many women of size will go on to develop one or more of the above-listed complications, some of these women will go on to experience completely normal pregnancies, labors and births. At the same time, some normal'or underweight'women will go on to develop significant morbidities not typically associated with women boasting BMIs less than 25.
For the professionals working with these women during (or, hopefully, before) theirpregnancies, the challenge becomes finding a way to communicate the gravity of these possibilities, without assuming every overweight expectant mother is a ticking time bomb, and all the while treating all expectant mothers with the best evidence-based care, no matter what their size.
[In tomorrow's installment of this series, we will look at some of the particular co-morbidities associated with maternal overweight/obesity, and the types of provider interactions and interventions that evidence does'and does not'support.]
Published: June 06, 2011
Tags
Maternal Infant CareCompassionate Care For Obese MothersEvidence-Based Care For Women of SizeGlobal Obesity EpidemicGlobesityRisks of Maternal ObesitySeries: Maternal Obesity From All Sides