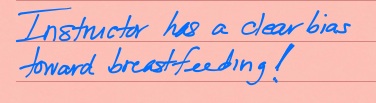
Instructor Has A Clear Bias Toward Breastfeeding!
By: Sharon Muza, BS, LCCE, FACCE, CD/BDT(DONA), CLE | 0 Comments
This post is part of a blog carnival in honor of World Breastfeeding Week. Honored to participate- SM
As it is World Breastfeeding Week and National Breastfeeding Month, my Google alerts, Facebook feeds and favorite blogs have been swirling with statistics, information, celebratory tidbits and fascinating facts about breastfeeding, locally, nationally and internationally.
In recognition of those people who support women who breastfeed, organizations are offering free access to journals and other resources during International Breastfeeding Week, including the International Lactation Consultant Association's free offer to download the quarterly, peer-reviewed Journal of Human Lactation, the US Department of Health and Human Services Office of Women's Health offering a free Breastfeeding Action Kit and the American College of Nurse Midwives' Journal of Midwifery and Women's Health offering free access to a past journal edition chock full of breastfeeding information.

Creative Commons Photo by ODHD
I think back to the breastfeeding relationship with my own two children, recalling my personal difficulties, struggles, trials, pain and tribulations that I slogged through while establishing a positive breastfeeding relationship with my first born and proving my own personal theory that we should always have our second children first! Remembering and appreciating the people who helped me to not give up, despite many setbacks, including many, many lactation consultants, my childbirth educator, my pediatrician, my local La Leche League support group, my partner, friends and family.
There has been a lot of press lately about expectations for women around breastfeeding. Several months ago, Time Magazine had an article entitled "Mothers' Milk" with a cover picture chosen specifically for its provocative nature. Recently, the American Academy of Pediatrics passed a resolution advising pediatricians not to provide formula company gift bags, coupons, and industry-authored handouts to the parents of newborns and infants in office and clinic settings. Nationwide, hospitals and two states (Rhode Island and just last month, Massachusetts) have banned the distribution of formula samples and bags, an action proven to increase breastfeeding rates. Even the Mayor of New York City, Mayor Bloomberg was getting in on the act recently, with his city's "Latch On NYC" campaign that limits access to formula by hospital staff among other things.
Most recently, I read a piece by Jane E. Brody, in the Personal Health section of The New York Times, titled "The Ideal and the Real of Breastfeeding," where Brody referenced a Scottish study, "A serial qualitative interview study of infant feeding experiences: idealism meets realism." (Hoddinott, Craig, Britten, 2012) published in the BMJ Open online journal. The researchers stated in their results and conclusions that;
Unanimously families would prefer the balance to shift away from antenatal theory towards more help immediately after birth and at 3-4 months when solids are being considered. Family-orientated interactive discussions are valued above breastfeeding-centred checklist style encounters.
Adopting idealistic global policy goals like exclusive breast feeding until 6 months as individual goals for women is unhelpful. More achievable incremental goals are recommended. Using a proactive family-centred narrative approach to feeding care might enable pivotal points to be anticipated and resolved. More attention to the diverse values, meanings and emotions around infant feeding within families could help to reconcile health ideals with reality.
Clearly, from the results of this study, and the recently released "Breastfeeding Report Card- United States, 2012," there is still a long way to go toward reaching the World Health Organization's recommendations that mothers worldwide "exclusively breastfeed infants for the child's first six months to achieve optimal growth, development and health. Thereafter, they should be given nutritious complementary foods and continue breastfeeding up to the age of two years or beyond."
Reading the Brody article and the referenced study brought me right back to when I worked for a major medical center in my community, as a childbirth educator, (I now teach independent classes) and my responsibilities included teaching a 2 1/2 hour breastfeeding class. This class, offered as part of a group package with other classes or available as a stand alone class, was well attended by both expectant mothers and usually their partners too.
I covered the usual topics, that I suspect pretty much any other breastfeeding instructor might hit upon, cramming a ton of information into the time allotted in the most interactive way possible. We talked about breast anatomy, how the breast makes milk, latch, positioning, feeding cues and needs of the newborn, potential problems, benefits, fears, when to reach out for additional support and specific resources in our community and so much more. Pumping, returning to work strategies and introducing a bottle were also covered. I recall sharing the preferred food for a newborn is its own mother's milk at the breast, pumped mother's milk, donor human milk and then artificial milk (formula) in that order. I explained that there are lots of ways to feed a newborn and I trust that each mother will find the way that works best for her and her baby.
Class evaluations were handed out at the end, and for years, I enjoyed the positive feedback and enthusiasm from the attendees, who stated time and time again that the class was fun, engaging and helpful, they felt more confident and should things be difficult, they knew they had resources for help. And then it happened. After years of teaching and hundreds and hundreds of students, I received an evaluation that struck me to the core. One that I still think about every time I teach breastfeeding classes or work with a birth doula client helping her and her newborn to get breastfeeding off to the right start. In blue pen, exclamation point included..."Instructor has a clear bias toward breastfeeding!"
 I felt like the air had been sucked out of the room. Left on the back table, in a pile of other evaluations, with no name or contact information. No way to follow up with someone who I clearly failed to connect with. Did I have a bias towards breastfeeding? It *was* a breastfeeding class. The objectives, as provided by the medical center had been met, but clearly, that night, I had not met a student's personal expectations. I felt horrible. And I still do, to this day.
I felt like the air had been sucked out of the room. Left on the back table, in a pile of other evaluations, with no name or contact information. No way to follow up with someone who I clearly failed to connect with. Did I have a bias towards breastfeeding? It *was* a breastfeeding class. The objectives, as provided by the medical center had been met, but clearly, that night, I had not met a student's personal expectations. I felt horrible. And I still do, to this day.
What were the expectations of this expectant mother from the breastfeeding class she signed up for? What pressures was she facing, from me, from others, that maybe I did not address, what fears or concerns did she (or her partner) have that I was not able to assuage? Did I "overpromote" breastfeeding? Breastfeeding is the biological norm for all mammals. It was a class to learn about breastfeeding her newborn. I went over every word I spoke that night in my mind, wondering if I crossed a line, even an invisible one that only she was aware of. Upon reflection, yes, I suppose I do have a bias towards breastfeeding. How could I not?
When I read all these articles, I feel like that line in the sand is being drawn all over again. How can birth professionals support the biologic norm while meeting new mothers where they are at? Providing support but not creating additional pressure. Set families up for success, but be ready to help them when the road is bumpy and even at times unsuccessful. How can we leave women feeling stronger after their breastfeeding experience, no matter how it goes down? How can we stand together with these new mothers, acknowledging what is best for babies, recognizing that all mothers inherently want to do their best and for reasons, sometimes within the mother's control and sometimes outside their control, things do not go as planned. Just like birth.
We must not leave mothers less than whole. For if we do, we do not create women who are well equipped to parent. We should stand united, supporting each other, teaching each other, letting children and young adults observe breastfeeding, talking about it to our peers, and co-workers and community. If I remember correctly, I never saw a baby breastfeeding, where I could observe closely, before I had my own children. I do not recall conversations with breastfeeding mothers, before I became an expectant parent, and we discussed breastfeeding in my childbirth class. We should not tolerate the sensationalistic articles published by attention grabbing media or be sucked in to their "feeding" frenzy, (pun intended) pitting one woman against another, forcing everyone to take sides.
I want to own that I do have a clear bias toward breastfeeding, but I want to support all women. Those that choose to breastfeed and those that don't. Or can't. I want to offer classes that are open and unbiased, provide accurate information and make myself accessible to all new mothers, who seek support, resources or just a listening ear and strong shoulder. I want a re-do with that mother in my class, so many years ago. I carry this unknown student's comment with me in every breastfeeding interaction I have. I also remember the wise words of my friend, colleague, mentor and hero, Penny Simkin; ""She has good reason for feeling this way, behaving this way, believing these things, and saying these things." I just may not know what those reasons are.
Please share with me, your thoughts on my experience. About your own "bias toward breastfeeding" and how you handle that with your students, clients and patients. I welcome respectful discussion and comments as we all celebrate and support women on their breastfeeding journey, whatever that looks like. - SM
References
Centers for Disease Control and Prevention , (2012). Breastfeeding report card-United States, 2012. Retrieved from website: http://www.cdc.gov/breastfeeding/data/reportcard.htm
Hoddinott P, Craig LCA, Britten J, et al. A serial qualitative interview study of infant feeding experiences: idealism meets realism. BMJ Open2012;2:e000504. doi:10.1136/bmjopen-2011-000504
Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database of Systematic Reviews 2002, Issue 1. Art. No.: CD003517. DOI: 10.1002/14651858.CD003517.
Published: August 03, 2012
Tags
BreastfeedingChildbirth educationMediaBreastfeeding SupportNewbornsMaternal Infant CareBabiesChildBirth In The MediaInfant Formula SamplesInfant NutritionTips For The ChildBirth Educator