Preconception and Women's Healthcare: An Interview with Dr. Michael Lu (Part One)
By: Walker Karraa, PhD | 0 Comments
Last April, I sat down with Dr. Michael C. Lu, director of the UCLA Preconception Care Clinic, lead investigator for Los Angeles County in the National Children's Study, and newly appointed Chair of the Secretary of Health and Human Services' committee on infant mortality. Dr. Lu is an associate professor of obstetrics and gynecology and public health at UCLA, and has been voted one of the Best Doctors in America since 2005. This five part series examines Dr. Lu's work in preconception health, and vision for maternal health care reform in the United States. At the end of this series, you will find a reference list of Dr. Lu's work, and links to presentations, and other articles of interest.
Preconception Care: An Introduction
Walker Karraa: Why is preconception health critically important to the new paradigm of prenatal care, and how would childbirth educators, advocates, and doulas benefit from learning more about it, and expanding their practices to include it?
Dr. Lu: I think what unites all of us is that we want healthy moms and healthy babies. And I'm glad people have more recently been talking about healthy dads, so really - healthy families. We may come from different backgrounds, different perspectives, different walks of life, but we're working for that common goal.
The question is how do we achieve that common goal? And when you look at most standard measures in this country, we're not doing great. In fact compared to most other developed countries, we're doing very poorly. How do we redesign the system, realign all the forces, so that we will engineer better teamwork, engineer better collaboration so that we can all achieve that same goal? We know we're missing a tremendous opportunity to optimize pregnancy outcomes by not doing better in terms of promoting preconception health and the life course perspective. For example the whole idea of allostatic load.
McEwen (2002) has this cartoon that explains allostasis and allostatic load beautifully:
Two kids balancing on the seesaw and maintaining the stability to change. But if you were to replace those two five kilogram kids with two five hundred kilogram sumo wrestlers, you put so much stress on the seesaw that sooner or later that seesaw's going to break. The wear and tear on the body over the life course from chronic biological or psychological stress - the body's allostatic systems become out of balance. We could be talking about in terms of immune system, endocrine system, about the metabolic system.

What if a pregnant woman were carrying these two five hundred kilogram sumo wrestlers on her back? You're not going to have a very good pregnancy. Prenatal care can try to get those two five hundred kilogram sumo wrestlers of her back, but we can't do it quickly enough to prevent pregnancy complications and to optimize fetal programming. If we really want to improve maternal and family health in this country, we have got to work on improving women's health and family's health before pregnancy - preconception care.
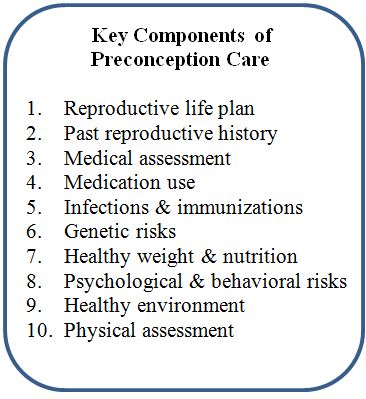
Walker Karraa: What are the components of a Reproductive Life Plan?
Dr. Lu: I think there's this conceptualizing and defining 'reproductive life plan' as a work in progress.
Currently it is proposed by many as simply asking every woman at every routine visit whether she wants to have any more children, and if so under what time frame, and what the clinician or provider can do to help her achieve her reproductive life plan.
Again it's a fairly narrow clinical approach, but it's a useful approach in that we're thinking more broadly and about the reproductive life plan: how do you get not just couples who are actively planning a pregnancy to think about their reproductive life plan, but how do you help those couples who had an unattended pregnancy to think about reproductive life plan before they had an unattended pregnancy. How do you help teenagers, or pre-teens to really think about reproductive life plan within their life's goals? So I think are still a lot of questions that we really haven't addressed in terms of how to conceptualize, how to define, how to promote reproductive life planning in the United States.
Walker Karraa: Do you think that a greater understanding of fetal programming would help?
Dr. Lu: I think it would really help. I had the fortune of sharing the lectern with Dr. David Barker over the last several years, and we have had a number of conversations where he really expressed a sense of frustration that the urgency of his message is still not quite getting out there.
Interestingly enough I was giving a talk for a nutritional organizational - talking with hundreds of registered dieticians in the audience. And when I asked them how many had heard about Barker Hypothesis, very few of them actually raised their hands. Given the central role of nutrition to fetal programming, if I were a registered dietician working in perinatal health, it would seem that all the work that I'd been doing had paid off - finally somebody's providing the scientific basis for why our work is so important! Barker's been doing this for 25 years and yet the message is not getting there.
Similarly I think in relation to Lamaze...given all the latest scientific evidence about fetal programming, and given the fact that Lamaze, and childbirth education in general is one of the most important sources of the information about pregnancy and childbirth that most American women have access to - I think there needs to be greater awareness and greater appreciation of what fetal programming means, and to really think about how childbirth education can be expanded to go beyond the components of educating about childbirth, epidurals, etc. To really think about how do we use the opportunity for childbirth education to really improve the health of women, children, and families, not only for those immediate birth outcomes but for their healthy well-being over the life-course.
Allen Rosenfield probably 30 years ago asked the question, 'Where is the 'M' in MCH?' Where's the 'mother' in maternal and child health programs - because much of MCH has focused on children's health and much less on maternal health. I think the question we're asking today is where's the 'W' in MCH - where's the woman in maternal and children's health? If we really want to improve maternal and child health in this country, we really have to start by improving women's health.
I think it's pretty much in alignment with what you're saying; it's not just about childbirth. If the natural childbirth movement is all about natural childbirth, it doesn't have the kind of impact that it could have. The focus should really be on promoting women's health over their life course continuum and how we would be a better society for doing that.
[Editor's note: In tomorrow's installment of this interview series, you will read further about preconception care and counseling, and Dr. Lu's proposal for an advancement of the practice of women's health care to become a '3.0 system' in which the obstetrician no longer resides at the center of the wheel. For a list of resources pertaining to this interview series, go here: resources and bibliography_dr lu interview series. ]
Published: July 18, 2011
Tags
PregnancyMaternal Infant CareAllostasisBarker HypothesisBarker TheoryDr. Michael LuNational Children's StudyPreconception CareReproductive Life PlanWomen's Health Care