Birth Outcomes by Birth Location: The Latest Study
By: Kimmelin Hull, PA, LCCE | 0 Comments
The much-anticipated Planned Place of Birth study out of the UK emerged last week in the British Medical Journal. As I complete a Biostatistics course for my Master's of Public Health ~ Maternal & Child Health program, I have to admit: this study, including the wealth of data contained herein, is a smorgasbord for statisticians. But for those who may not feel naturally inclined toward margins of errors and confidence intervals, interpreting the results of such a study might feel more like a nightmare. While the blogosphere has been philosophically abuzz about this new segment of data looking at the safety of childbirth practices by location, I would like to take a look at this study from a statistics perspective. In the coming days, we will have another review of this study submitted by evidence-based maternity care expert, medical writer, and speaker Henci Goer.
The study by the Birthplace in England Collaborative Group, Perinatal and Maternal Outcomes by Planned Place of Birth for Healthy Women in Low Risk Pregnancies, is a prospective cohort study conducted through the National Perinatal epidemiology Unit at the University of Oxford. You may recall that a prospective cohort study is an observational, forward-looking study that follows one or several groups of subjects over a specified period of time. No assigned interventions or treatments took place as would be typical in a clinical trial. The overall objective of this study was
"to compare perinatal outcomes, maternal outcomes, and interventions in labour by planned place of birth at the start of care in labour for women with low risk pregnancies.'
The study authors explain that this study was conducted in response to several others in recent years that aimed to examine the risks and benefits associated with childbirth, relative to location, but failed to assign study groups based on planned rather than eventual place of birth. The ultimate goal of the current study, then, was to
"compare intrapartum and early neonatal mortality and specific neonatal morbidities for births planned at home...'
...in the locales detailed below. To me, this study feels a bit similar to a case-control study as odds ratios are used extensively in the data to determine the likelihood of certain events occurring during the observed births in relation to the birth location. (Odds ratios are commonly computed for the data of case-controlled studies.)
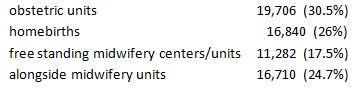
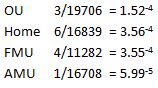
This study included 64,538 women who gave birth between April 2008 and April 2010 in the UK, and were segmented (not by researchers, but previously by patient choice) into one of four categories: homebirth, free-standing midwifery centers, 'alongside' midwifery units (midwife-attended birth centers within a hospital), and in-hospital obstetrics units. Remember: these locations pertain to pre-labour planning and initiation of intrapartum care in terms of where the woman/couple intended to give birth. The number of birthing women in each subgroup were as follows:
As the data was collected and assimilated, further stratification of the data took place: 1) assessing outcomes of nulliparous vs. multiparous women and 2) women who did, or did not, have a 'complicating condition' at the start of care in labor. These complicating conditions included:
| prolonged rupture of membranes |
hypertension |
| amniotic fluid meconium staining |
abnormal vaginal bleeding |
| proteinuria |
abnormal fetal heart rate |
| non-cephalic fetal presentation |
|
Women who underwent elective cesarean sections or unplanned homebirths, as well as those who were not considered 'low risk' as defined by the National Institute for Health and Clinical Excellence (NICE) guidelines, were excluded from this study. These exclusions can be seen as helpful or hindrance, depending upon the results one is interested in. By deleting planned cesareans, there is some difficulty in being able to completely generalize the results of the data to the whole population where elective cesareans do, of course, take place - including their inherent ratios of primary and secondary outcomes. However, in an effort to assess outcomes ofspontaneous labor and delivery outcomes, it makes sense to exclude this data. Excluding unplanned homebirths, on the other hand, makes perfect sense to me as most of these types of births are unattended by any sort of maternity care provider, and therefore not applicable in this study design.
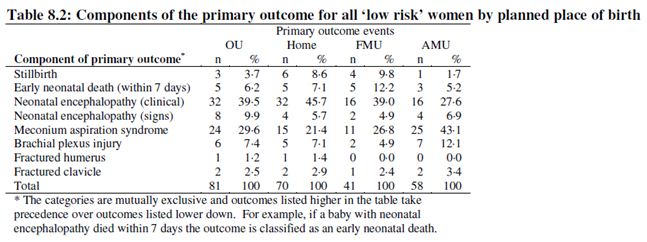
Outcomes assessed were broken down into primary and secondary outcomes as follows:
| Primary outcomes included*: |
|
| Intrapartum stillbirth |
meconium aspiration syndrome |
| Early neonatal deaths |
brachial plexus injury |
| Neonatal encephalopathy |
fractured humerus or clavicle |
| Secondary outcomes included*: |
|
| spontaneous vertex birth |
syntocin augmentation |
| ventouse delivery |
immersion in water for pain relief |
| forceps delivery |
epidural or spinal analgesia |
| intrapartum c-section |
general anesthesia |
| 3rd or 3th degree perineal tear |
no active management of third stage |
| blood transfusion |
episiotomy |
| admission to higher level of care |
|
*notice, outcomes such as maternal mortality, postpartum hemorrhage and postnatal mood disorders are not included here.
(To access all data tables for this study, go here.)
The summarized results from the study are as follows:
The overall 'primary outcomes' incidence for the entire study population was 4.3/1000 births (95% confidence interval of 3.3/1000 - 5.5/1000) Remember, a confidence interval tells us that we are 95% sure that the true incidence of primary outcomes in the studied population, as predicted by the study data - the 'point estimates' - likely falls in the interval of 3.3-5.5/1000 births.) The incidences for each subgroup were as follows:
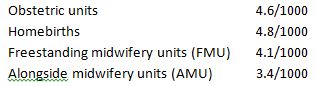
And from the study, a summary of the findings, per group, are as follows:
We are also given odds ratios to go along with these figures - helping us to recognize the significance of the primary outcomes, in relation to location of birth. In essence, an odds ratio greater than 1.0 suggests that 'exposure' to a variable of interest (in this case, place of birth) isa risk factor for the outcome(s) of interest. An odds ratio less than 1.0 suggests that exposure isprotective against the outcome(s) of interest. An odds ratio close to 1.0 suggests no significant associations between exposure and outcome. Knowing this, let's look at the (adjusted) odds ratios from this birth place study:

With all these numbers hovering rather close to 1.0 (with the exception of the alongside midwifery units boasting an odds ratio of less than 1.0) we can conclude that birth place may only bear a small amount of responsibility for primary outcomes - as defined in this study - in the homebirth group; negligible effect on the obstetric unit and FMU groups; and a protective effect on the AMU group. In fact, the study authors concluded that,
"Overall, there were no significant differences in the adjusted odds ratios of the primary outcomes for any of the non-obstetric unit settings compared with obstetric units.'
Perhaps the implications made by the adjusted odds ratios would be a bit more powerful, if the study group sizes were more equal (see numbers and percentages of groups above). And yet, for such an impressively large study, the distribution of the study population amongst the four groups is also rather impressive, considering the distribution of birth locale in the general population, as supplied by study authors: 92% of births in the UK occur within obstetric units and just 8% outside (2.8% at home; 3% in AMUs and <2% in FMUs).
The most striking outcome that anti-homebirth writers are citing as cause for alarm are the numbers for stillbirths, as delineated in the following table:
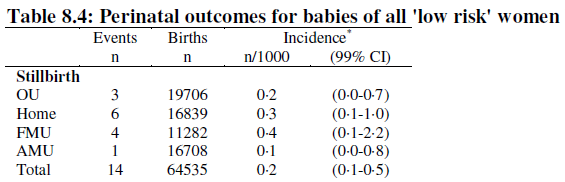
If you just look at the crude numbers, you will conclude that babies born at home are twice as likely to die during the birth process, compared to babies born in obstetric units. Perhaps in some places around the world, this might be a very real estimate. But in this study, we need to remember the difference in subgroup sizes: there were 2,866 more births in the obstetric units group than in the homebirths group, for example. So, if we instead look at the incidence of stillbirth between the groups, we get a different picture:

Now, I'm not going to sit here and suggest that even the difference between 0.2 and 0.3 stillbirths/1000 is insignificant... it's certainly not to the additional three the families who experienced those outcomes. I don't think anyone should ever make that claim from an individual perspective. But, if looking at the data from a statistics perspective - the perspective that informs us when we are advising expectant women/couples on place of birth... or when making our own decisions about birth locale - the incidences are still very low: out of the 16,839 homebirths, the stillbirth ratio for each group was:
Some other interesting numbers that came out in the data are as follows:
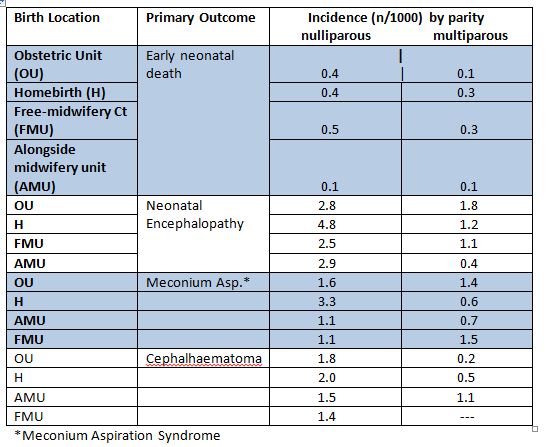
The above data suggests that the differences in outcomes between first time (nulliparous) mothers and subsequent (multiparous) mothers are more favorable for women who've undergone childbirth previously - regardless of birth location. The study authors summarize these findings, in terms of policy implications, this way:
'Adverse perinatal outcomes are uncommon in all settings, while interventions during labour and birth are much less common for births planned in non-obstetric unit settings. For nulliparous women, there is some evidence that planning birth at home is associated with a higher risk of an adverse perinatal outcome.'
After reading the study and the statistics, what do you think???
~ Stay tuned for more coverage of this study ~
Posted by: Kimmelin Hull, PA, LCCE, FACCE
Published: November 29, 2011
Tags
HomebirthHospital BirthLamaze InternationalLamaze EducatorsLabor/BirthMaternal Infant CareLamazeOnline StoreChildBirth Research From Oxford UniveristyPlace Of Birth StudyRates StillBirth