Assessing Birth Settings to Improve Value and Optimize Outcomes in U.S. Maternity Care
By: Sharon Muza, BS, LCCE, FACCE, CD/BDT(DONA), CLE | 0 Comments
by Wendy Gordon, CPM, LM, MPH, MANA Division of Research, Assistant Professor, Bastyr University Dept of Midwifery
Today, occasional contributor, midwife and researcher Wendy Gordon, LM, CPM, MPH, Midwives Alliance Division of Research, shares some insights into some of the fascinating discussions that took place at last week's Institute of Medicine's workshop focusing on birth place settings. From all reports from the many people in attendance, this workshop will hopefully help move the research and discussion on the topic of birth place settings forward and create opportunities for more families to chose to birth where they feel most comfortable and safe. ' Sharon Muza, Community Manager, Science & Sensibility

Hannah Russell-Davis nurses her newborn son
©photo by Michael Davis http://getprivatepractice.com
Last week marked an historic opportunity for maternity care providers to regroup and become inspired to move our professions forward together in all birth settings. The two-day event, hosted by the prestigious Institute of Medicine (IOM) and sponsored by the W.K. Kellogg Foundation, focused on 'Research Issues in the Assessment of Birth Settings' and brought together the greatest minds in research and practice in all three birth settings: home, birth center and hospital. Issues of tremendous importance to consumers, providers and researchers in the birth community were discussed in a collegial and inspiring manner- marred only by one presentation that stirred a bit of controversy.
Historic Workshop Can Positively Impact Future Research
Similar to the first IOM conference on this topic over 30 years ago, the intent of last week's gathering was to discuss the research regarding the effect of place of birth on maternal and infant outcomes. Invited speakers included researchers, public health professionals, midwives, nurses, pediatricians and obstetricians. In structured mini-sessions, panelists shared their expertise on the following topics:
- the historical and current picture of who is giving birth in the different settings;
- definitions of 'low-risk' versus 'high-risk';
- what the best research says about safety in various settings;
- education, regulation and management of different types of providers;
- methods of collection and use of data regarding maternity care and birth in various settings;
- cost and value differences between settings and reimbursement issues; and
- the rich and varied perspectives of providers in the three childbirth settings.
Members of the audience were just as impressive as the panelists themselves when, at the end of each panel, the microphone was opened and significant content was added through their questions and comments.
A lot of ground was covered over the course of the two days, and there were several takeaways that had particular impact for the midwifery community. The home birth rate in the U.S. was predicted to continue its rise with the next release of CDC data, reaching about 31,500 births nationwide in 2010. The MANA Stats web-based system was touted by attendees as the best data collection system for home birth outcomes. Birth certificate data was shown to still have major problems in its ability to accurately capture intended place of birth and other reliability issues, despite improvements in recent years. A Medicaid study from Washington State demonstrated vast cost savings with midwifery care and birth at home and in birth centers. The workshop report will have tremendous potential to impact contemporary birth policy and research agendas.
Lack of Consumer Representation and Little Discussion of Health Disparities
There was no consumer representation on workshop panels, nor was there a panel addressing disparities in maternal and infant outcomes, which seems to have been a grave oversight of the organizers. In the 30 years since the last IOM workshop on birth settings, overall infant mortality has been reduced from 11.5/1000 to 6.7/1000, but the black-white gap has actually increased. In 1982, nearly twice as many babies born to black mothers than white mothers died before their first birthday (19.6 infant deaths per 1000 births vs 10.1/1000; National Center for Health Statistics, 1986). Recent mortality figures show that disparity to be even wider (12.67/1000 vs 5.52/1000; Mathews & MacDorman, 2012).

Hannah Russell-Davis holds her
son Jack, moments after his birth
at their home in Charlottesville,
VA. Jack was Hannah's third home birth.
© photo by Michael Davis
http://getprivatepractice.com
With childbirth in home and birth center settings gaining momentum nationally and at the state level, research to support policy in this direction is more important than ever. The best research has shown for decades, and continues to show, that for women with low-risk pregnancies, birth that is planned to occur in the home and birth center settings with a skilled midwife is no more risky than birth in the hospital and results in far fewer interventions, lower cost and higher satisfaction (Vedam et al, 2012). Hopefully, the breadth of this research can finally start to expand beyond proving that it is safe.
'Recrudescence' Revisited
Despite this body of literature, there are still some physicians who persist in torturing the data in an attempt to frame their personal opinions as 'science.' It was disappointing, although perhaps not surprising, to see Dr. Frank Chervenak use his time on the provider panel to do just that. The American Journal of Obstetrics and Gynecology recently published an article authored by Dr. Chervenak regarding the 'recrudescence of homebirth' (Chervenak et al, 2013), and perhaps it was the controversy stirred by that article that prompted the conference organizers to invite him to speak on this panel. The panel members included Dr. Chervenak as a hospital-based provider, Karen Pelote, CNM with the birth center provider perspective, and Brynne Potter, CPM as a homebirth provider. Both Pelote and Potter appeared to have taken seriously the purpose of their panel representation and showcased the data on our client-centered models of care, with photos and quotes from women regarding the care they received and their experiences in the birth center and home settings.
In stark contrast, Chervenak used his 12 minutes (out of 10) that were to be devoted to the hospital provider perspective for, instead, a rapid-fire display of 'back-of-the-envelope' bar graphs attempting to show home/hospital differences in 5-minute Apgar scores using raw data drawn from birth certificates. Since it appears that some doctors are having a hard time getting their 'research' on this topic published in peer-reviewed journals, they are presenting their data in settings that do not require peer-review, such as last year's annual conference of the Society of Maternal-Fetal Medicine (the study still hasn't been published) and this IOM workshop. Meanwhile, there are several well-designed studies published in peer-reviewed journals that show that there is no difference in 5-minute Apgar scores between home and hospital settings (Hutton et al, 2009; Janssen et al, 2009; van der Kooy et al, 2011).
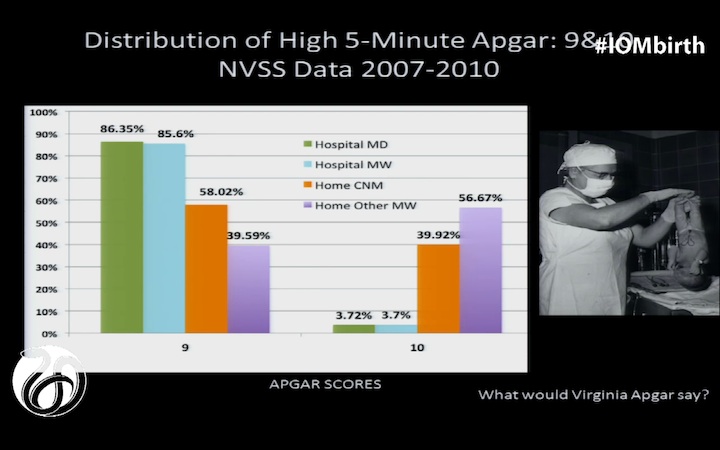
Apgar Distribution Hospital vs. Home © Dr. Frank Chervenak 2013
That a professional invited to contribute to a high-level workshop about research would present an un-peer-reviewed thesis based on unreliable data, lacking any statistical analysis, is'¦ well, let's just say 'puzzling.' Exploiting the concept of 'relative risk,' Chervenak sliced and diced the data in more ways than were thought possible to suggest that babies born at home were more likely to have a low 5-minute Apgar score than babies born in the hospital.
'Home Births Should Not Happen'
Chervenak's non-reviewed data did find a higher rate of Apgar scores of '10' in the home setting versus '9' in the hospital setting. His point? Not that, clinically speaking, there is no difference between a score of 9 vs. 10 (they're both good). Not that babies might possibly be doing better due to normal physiologic labor and undisturbed birth and that we should explore this further. Instead, he suggested ' at this historic setting ' that midwives lie about Apgar scores because 'no one is watching.' After a day and a half of earnest, interprofessional collegiality, Chervenak wrapped up his extended presentation with his unabashed opinion: 'Home births should not happen.'
Epidemiologists in the room were quick to step to the microphone for the open discussion part of the panel, pointing out the many flaws in Chervenak's presentation. Marian MacDorman, Ph.D., senior statistician and researcher for the CDC's National Center for Health Statistics, reminded everyone that birth certificate data is notoriously unreliable for neonatal seizures and low Apgar scores; this has been shown time and again for decades and had indeed been discussed earlier in this very workshop. More importantly, McDorman stated that data from birth certificates cannot be used to make comparisons between settings or providers. Her point, which deserves some elaboration here, is that there is a very important distinction between 'absolute risk' and 'relative risk,' and different types of data are better than others depending on what you are trying to describe.
'When we limit access to certain birth settings because of risk, are we examining the risks of the alternative?' ' Brynne Potter, CPM
Absolute vs. Relative Risk
Let's say that a person's odds of getting struck by lightning in a heavily populated city are one in a million, and those same odds in a rural area are five in a million. These odds are called your 'absolute risk' of being struck by lightning. Another way to look at this is to say that a person's odds of being struck by lightning are five times higher in a rural area than in a densely-populated area; this is the 'relative risk' of a lightning strike in one area over another.
A common approach of anti-homebirth activists is to use the 'relative risk' approach and ignore the absolute risk, because it's much more dramatic and sensationalistic to suggest that the risk of something is 'double!' or 'triple!' that of something else, even though the absolute risk of those things are very low and may not even be statistically significantly different from each other. Of course, any infant or maternal mortality is a tragedy. But one of the key points raised at the IOM workshop was the idea that, in our efforts to identify 'safety' with one indicator (mortality) or 'truly low-risk' pregnancies by their absence of a particular factor (breech position, for example), we often fail to quantify all of the impacts of the various settings in ways that are meaningful to the women who experience the outcomes, such as the fact that in many areas, the only option for breech delivery is cesarean or the only way a VBAC can happen is at home, attended or not. As Brynne Potter asked last week: when we limit access to certain birth settings because of risk, are we examining the risks of the alternative?
To return to the lightning analogy, it would be deeply disingenuous for a person to say that you shouldn't move to a rural area simply because your risk of being struck by lightning is five times higher, without mentioning that at worst, that risk is five in a million. The ethics of this are further called into question when the person suggesting this is a trusted care provider, and is even worse when that person withholds all information about your option to move to a rural area ' disregarding all of your other reasons for wanting to doing so ' because they have decided that the risk of being hit by lightning there is too high for you.
Clarifying the Validity of Birth Certificate Data
Dr. MacDorman clarified how to interpret the data for anyone who might have been misled by Dr. Chervenak's slides. She pointed out that regarding low Apgar scores, 'the absolute risk is low; that's all you can say with vital data.' It doesn't happen very often in any setting; most studies on homebirth around the world report the occurrence of low Apgar scores (<7) in the range of 1%, and very low scores (<4) are even rarer. Studies have shown that the more rare an occurrence is, the less likely it is to be captured accurately on the birth certificate (Northam & Knapp, 2006).
Overall, the Midwives Alliance Division of Research (DOR) and other organizations working to improve maternity care are pleased with the near-consensus viewpoint by the majority of the disciplines represented at this workshop: that normal physiologic birth is best for mother and baby and should be the goal of all settings and practitioners. We are looking forward to the future research inspired by this event. We believe that there is potential for there to be more movement in the next 30 years than there was since the last IOM workshop on this topic 30 years ago, particularly because of the availability of high-quality datasets such as MANA Stats (primarily planned home births) and the American Association of Birth Centers' Uniform Data Set (primarily planned birth center births). As the stewards of the largest database on midwifery care and outcomes of normal physiologic birth in the home setting, the DOR encourages researchers to apply for the MANA Stats data to conduct this important research (application information at mana.org/DOR).
References:
Chervenak FA, McCullough LB, Brent RL, Levene MI, Arabin B. 2013. Planned home birth: The professional responsibility response. AJOG 208(1):31-38.
Hutton EK, Reitsma AH, Kaufman K. 2009. Outcomes associated with planned home and planned hospital births in low-risk women attended by midwives in Ontario, Canada, 2003-2006: A retrospective cohort study. BIRTH 36(3):180-189.
Janssen PA, Saxell L, Page LA, Klein MC, Liston RM, Lee SK. 2009. Outcomes of planned home birth with registered midwife versus planned hospital birth with midwife or physician. CMAJ, doi:10.1503/cmaj.081869.
Mathews, TJ & MacDorman, M. 2012. National Vital Statistics Reports: Infant mortality statistics from the 2008 period linked birth/ infant death data set. Available online at http://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_05.pdf.
National Center for Health Statistics. 1986. Vital Statistics of the United States, 1982, Vol II: Mortality, Part A. DHHS Pub. No. (PHS) 86-1122. Public Health Service: Washington. U.S. Government Printing Office.
Northam S, Knapp TR. 2006. The reliability and validity of birth certificates. J Obstet Gynecol Neonatal Nurs 35(1):3-12.
van der Kooy J, Poeran J, de Graaf JP, Birnie E, Denktas S, Steegers EAP, Bonsel GJ. 2011. Planned home compared with planned hospital births in the Netherlands: Intrapartum and early neonatal death in low-risk pregnancies. Obstet Gynecol 118:1037-46.
Vedam S, Schummers L, Stoll K, Fulton C. 2012. Home Birth: An Annotated Guide to the Literature. Available online at http://mana.org/DOR/research-resources/.
About Wendy Gordon
 Wendy Gordon, LM, CPM, MPH is a midwife, mother and educator in the Seattle area. She helped to build a busy, blended homebirth practice of nurse-midwives and direct-entry midwives in Portland, Oregon for eight years before recently transitioning to Seattle. She is a Coordinating Council member of the Midwives Alliance Division of Research, a board member of the Association of Midwifery Educators, and teaches at the Bastyr University Department of Midwifery.
Wendy Gordon, LM, CPM, MPH is a midwife, mother and educator in the Seattle area. She helped to build a busy, blended homebirth practice of nurse-midwives and direct-entry midwives in Portland, Oregon for eight years before recently transitioning to Seattle. She is a Coordinating Council member of the Midwives Alliance Division of Research, a board member of the Association of Midwifery Educators, and teaches at the Bastyr University Department of Midwifery.
Published: March 12, 2013
Tags
HomebirthMidwivesLabor/BirthBirth CentersMaternal Infant CareInstitute Of MedicineMarian MacDormanMANAChervenakWendy GordonApgarBirth SettingBrynne PotterFrank ChervenakKaren Pelote